A 48 year old female with complaint of shortness of breath.
Welcome and greetings to every one who are visiting my blog. This is an online E log platform to discuss our patient's de-identified health data shared after taking his/her/guardian's signed, informed consent. I have been given this case in order to solve in an attempt to understand the topic of patient's clinical data analysis to develop my competency in reading and comprehending clinical data and come up with a diagnosis and treatment plan.
CHIEF COMPLAINT:
A 48 year old female, resident of Hyderabad and home -maker by occupation, came to casualty on 14/3/22 with complaints of :
-shortness of breath 2 week back - initially grade -2 later progressed to grade 4 .
-pedal edema and chest tightness
-generalized weakness and fatigue and frequent falls
-difficulty opening mouth and oral ulcers 2week back.
-difficulty in swallowing both solids and liquids since 10 days .
-H/O skin peeling all over body 35 DAYS ago .
HOPI:
Patient's timeline



-5 months back patient visited hospital for arthralgia and was diagnosed with type2 DM. She did not take any medications for it.
-2 months back patient was on ATT i.e. Jan1 2022 as she was diagnosed with miliary tuberculosis.
-1 month back ATT was stopped, she developed scleroderma secondary to ATT. She was kept under supportive management and recovered in 20 days.
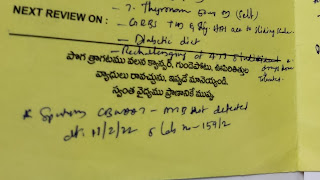
SPUTUM CBNAAT REPORT - OUTSIDE HOSPITAL.
PERSONAL HISTORY :
loss of appetite
weight loss present
sleep adequate
bowel and bladder movements regular
C/O burning micturition since 1 week
GENERAL EXAMINATION :
The patient is conscious coherent and cooperative and well oriented to time and place.
PALLOR - PRESENT
NO ICTERUS ,CYANOSIS ,CLUBBING ,LYMPHADENOPATHY
MILD EDEMA - NON PITTING EXTENDING UPTO FEET .
VITALS:
The patient is conscious coherent and cooperative and well oriented to time and place.
PALLOR - PRESENT
NO ICTERUS ,CYANOSIS ,CLUBBING ,LYMPHADENOPATHY
MILD EDEMA - NON PITTING EXTENDING UPTO FEET .
VITALS:
Temperature:100F
PR: 98bpm
PR: 98bpm
BP:130/80mm Hg
RR:27cpm
Spo2: 95%
GRBS:105gm%
HEAD TO TOE EXAMINATION :
RR:27cpm
Spo2: 95%
GRBS:105gm%
HEAD TO TOE EXAMINATION :
-ALOPECIA- PRESENT.
-EYES - Proptosis Seen . NO conjunctival suffusion
-EOM- intact
-MICROSTOMIA PRESENT
-BALD TONGUE NOTED , RED COLOR
-no ulcers .
-THYROID- no goitre noted
SKIN -
-MULTIPLE HYPER- PIGMENTED MACULES SEEN ALL OVER FACE, UPPER LIMBS,NECK, THIGH, ABDOMEN AND UPPER BACK .
-DRY SKIN PRESENT
-THICKENING OF SKIN over fore arms , dorsum of hand and fingers and on around mouth.
-absent hair
-SLIGHT PEELING still over arms and legs .
SYSTEMIC EXAMINATION :
RS:
-Inspection :
Movements of chest appears to be Equal on both sides .
-Palpation vocal fremitus decreased in left mamary , ISA area
-Percussion: Dull note in left mamary area and ISA .
-Auscultation : Decreased air entry on left ISA,IMA .
RIGHT side - normal air entry .
-BILATERAL VESICULAR BREATHING NOTED .
-Tubular breathing heard on right inter-scapular area .
-Coarse crepitations - end inspiratory - no variation with cough - heard on left ISA >>right ISA .
RS:
-Inspection :
Movements of chest appears to be Equal on both sides .
-Palpation vocal fremitus decreased in left mamary , ISA area
-Percussion: Dull note in left mamary area and ISA .
-Auscultation : Decreased air entry on left ISA,IMA .
RIGHT side - normal air entry .
-BILATERAL VESICULAR BREATHING NOTED .
-Tubular breathing heard on right inter-scapular area .
-Coarse crepitations - end inspiratory - no variation with cough - heard on left ISA >>right ISA .
CVS:
S1S2 heard.
No murmurs. No palpable heart sounds.
PER ABDOMEN :
SOFT , NO ORGANOMEGALY.
S1S2 heard.
No murmurs. No palpable heart sounds.
PER ABDOMEN :
SOFT , NO ORGANOMEGALY.
NO GUARDING AND RIGIDITY.
BOWEL SOUNDS PRESENT .
CNS :
NO FOCAL NEUROLOGICAL DEFICITS .
GAIT - NORMAL
RHOMBERGS NEGATIVE .


BOWEL SOUNDS PRESENT .
CNS :
NO FOCAL NEUROLOGICAL DEFICITS .
GAIT - NORMAL
RHOMBERGS NEGATIVE .





INVESTIGATIONS:
RBS: 70mg/dl
HbA1c : 6.8%
RFT:
Blood Urea: 136mg/dl
S. Creatinine: 4.8mg/dl
Na 139
K 3.0
Cl 102
Hemogram:
HB 7.2
TC 15,000
MCV 80.4
PCV 21.5
MCH 27.0
MCHC 33.6
PLT 3.67
RDW 62
P.S NORMOCYTIC, NORMOCHROMIC
Serum iron : 45ug/dl
ABG:
pH 7.34
PCo2 18.8
PaO2 92.4
HCO3 12.2
SpO2 96
LFT:
TB 2.8
DB 0.74
AST 14
ALT 10
ALP 673
TP 7.4
ALB 2.23
CUE:
ALB ++
Sugars nil
Pus cells plenty
Epithelial cells 1-2
COVID-19 RAT - NEGATIVE
ESR - 180
CRP - POSITIVE (1.2 mg/dl)
RA FACTOR - NEGATIVE .
LDH - 326 IU/L
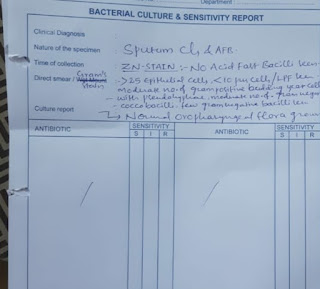
REPEAT SPUTUM AFB OUT HOSPITAL REPORT :
( 19/03/22)
Chest X-ray:

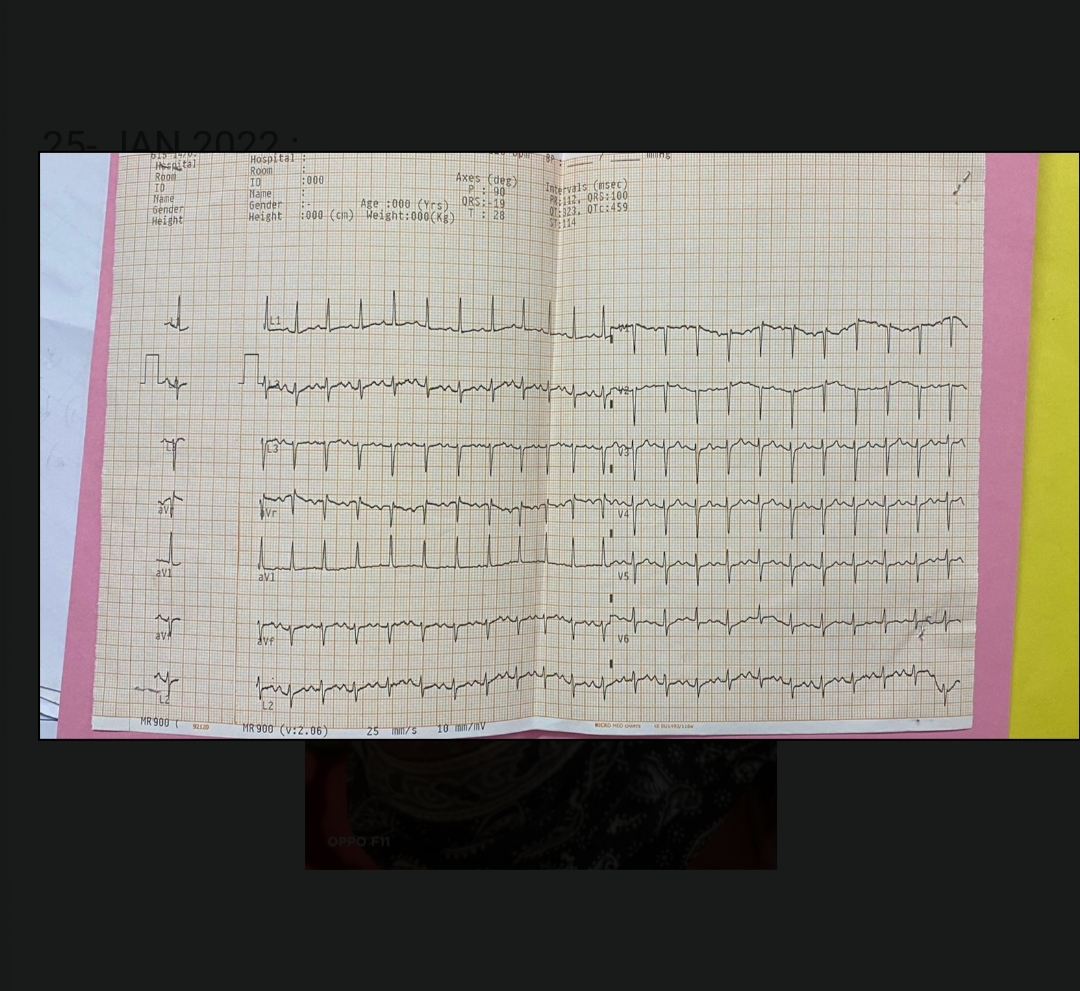
ECG:
USG ABDOMEN:
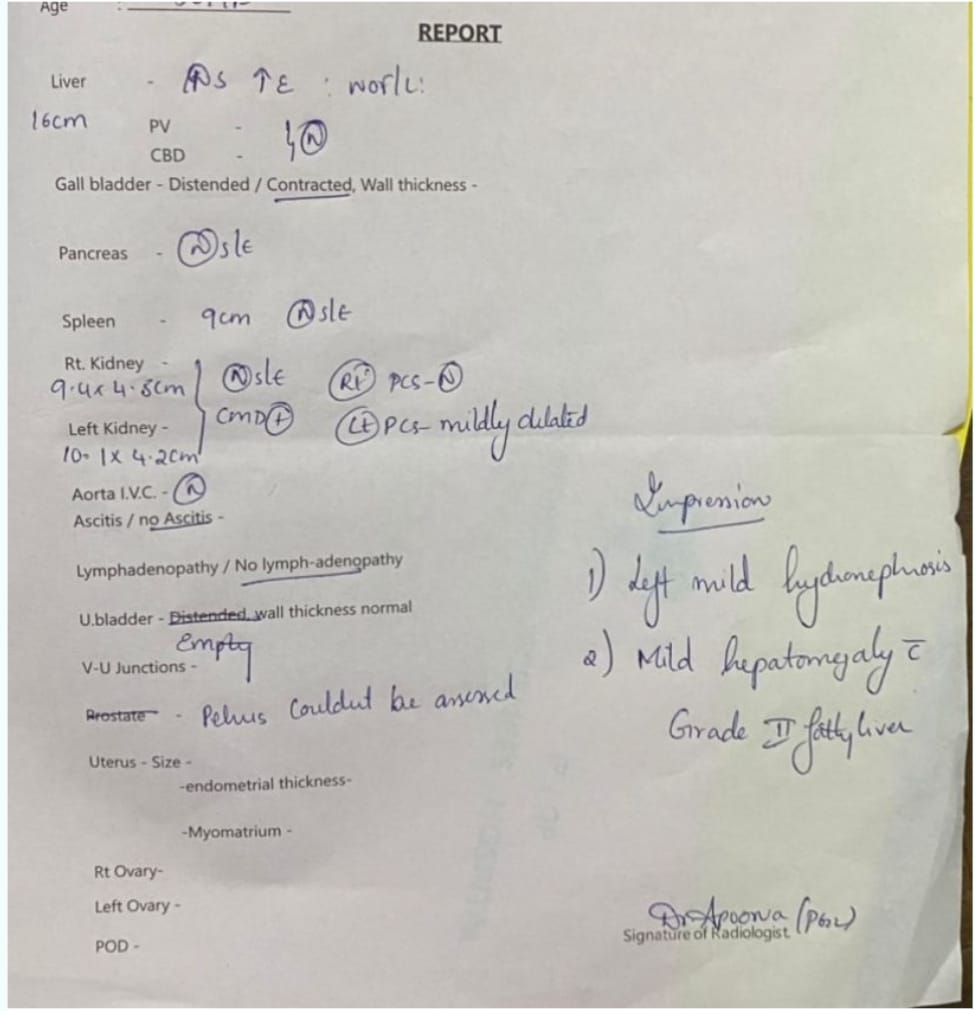
USG IMPRESSION: LEFT MILD HYDRONEPHROSIS AND MILD HEPATOMEGALY WITH GRADE2 FATTY LIVER.
High resolution computed tomography:
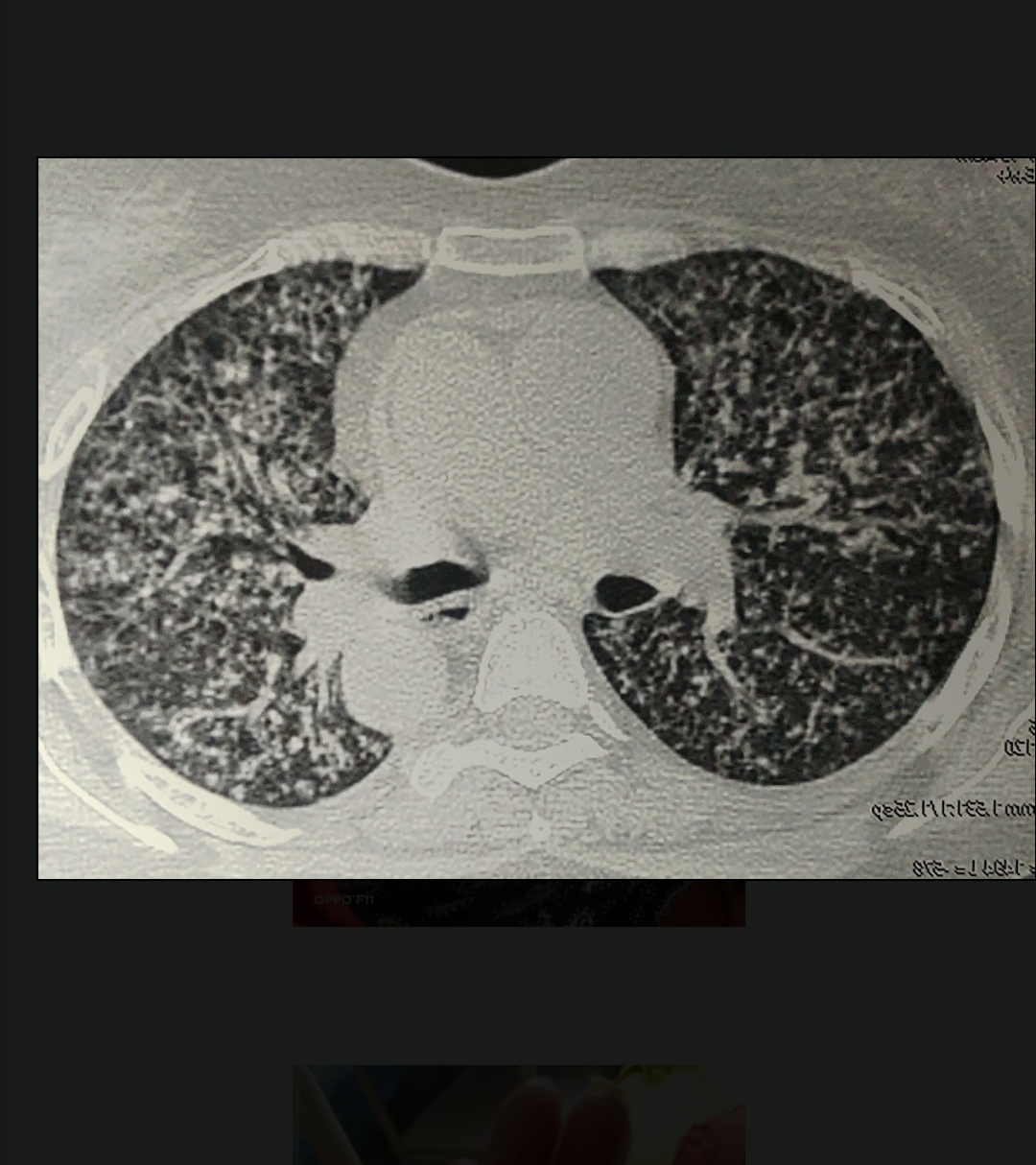
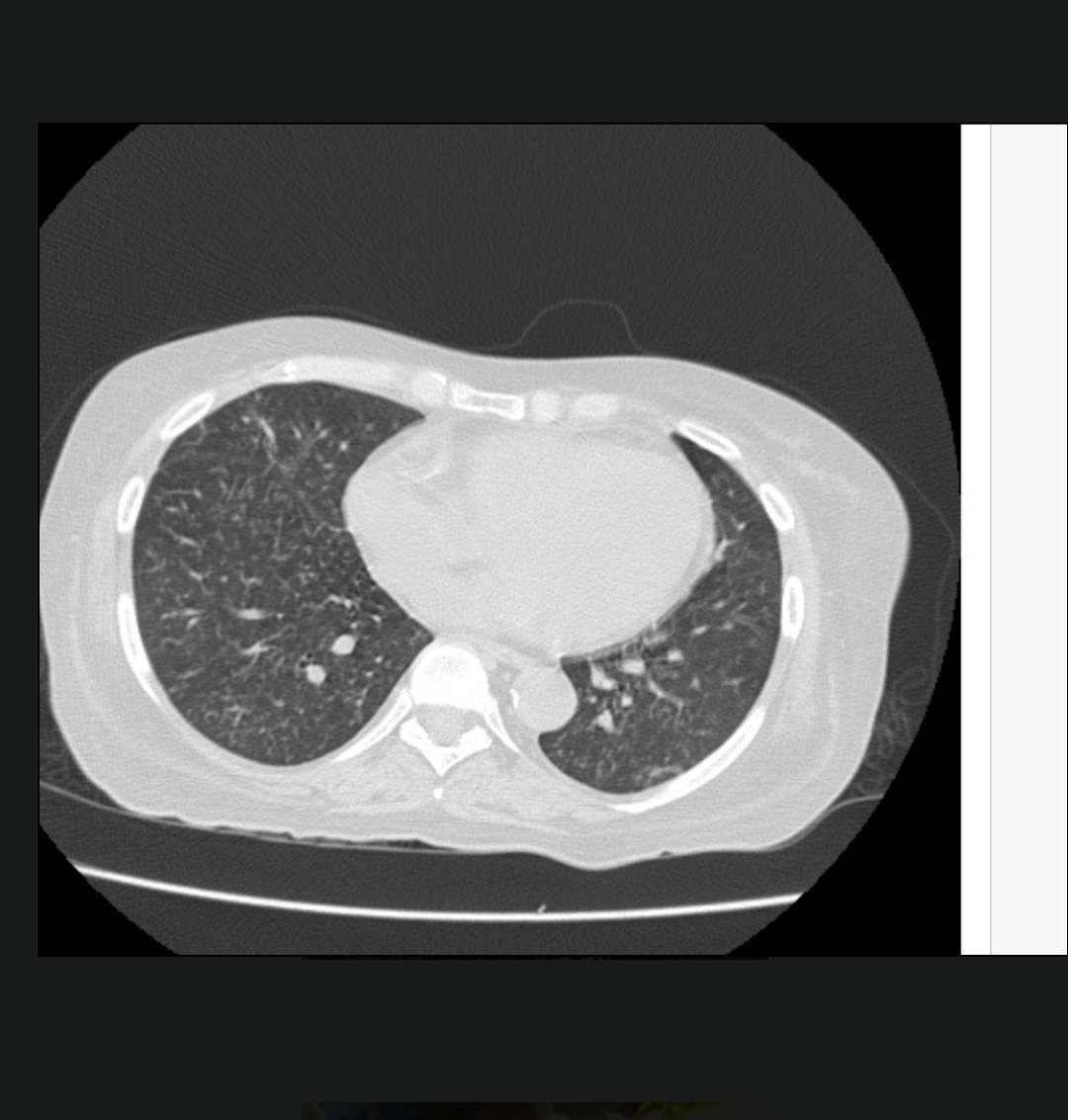
-Few small volume mediastinal lymph nodes noted
-Both lungs are studded with tiny nodular densities - miliary TB or ILD?
-Small air filled cyst noted left lower lobe.
-No evidence of effusion.
-Non-obstructive left renal calculus.
PROVISIONAL DIAGNOSIS :
Miliary tuberculosis , ATT induced scleroderma
K/c/o HTN , HYPOTHYROIDISM
TREATMENT PLAN:
High resolution computed tomography:
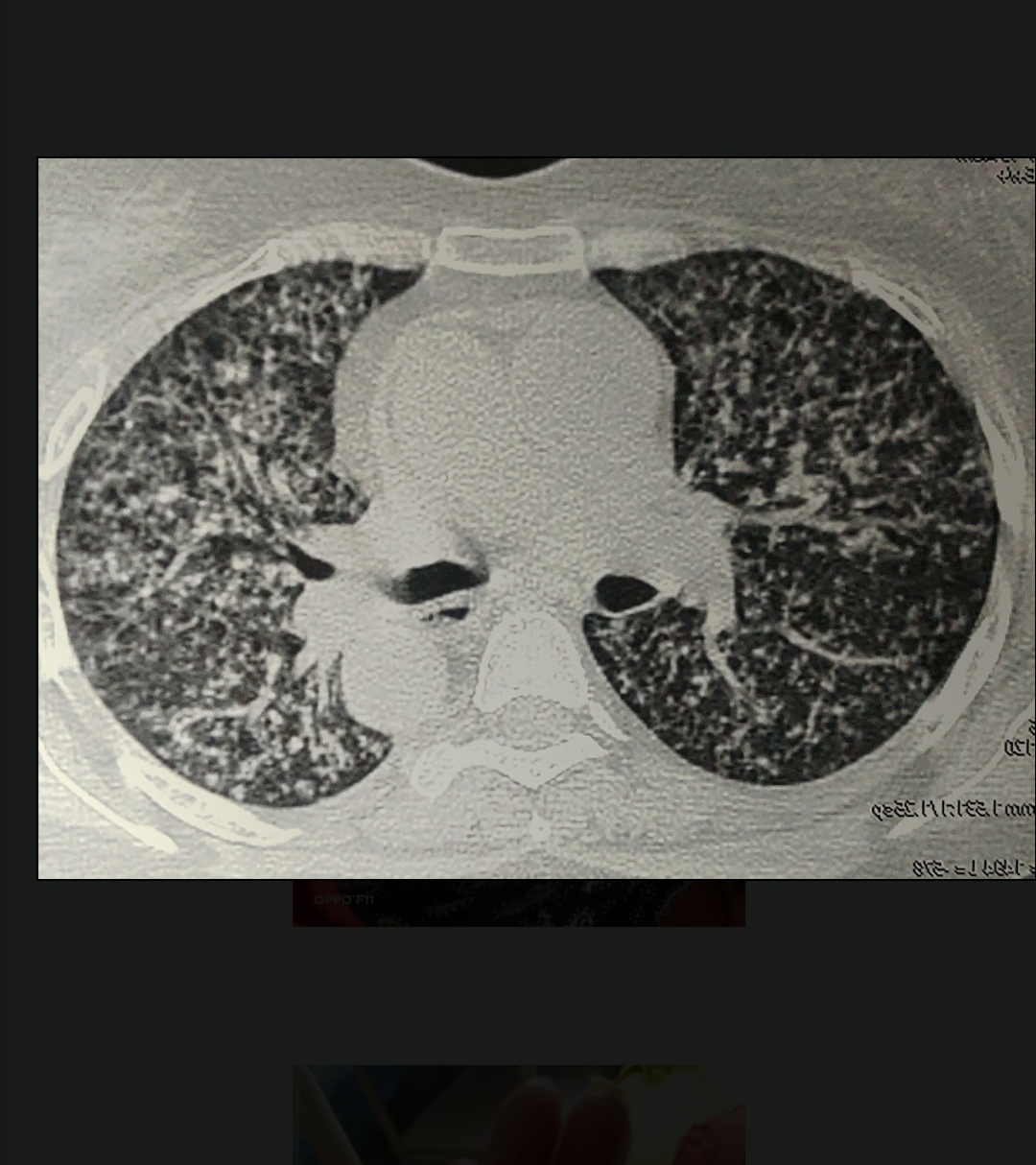
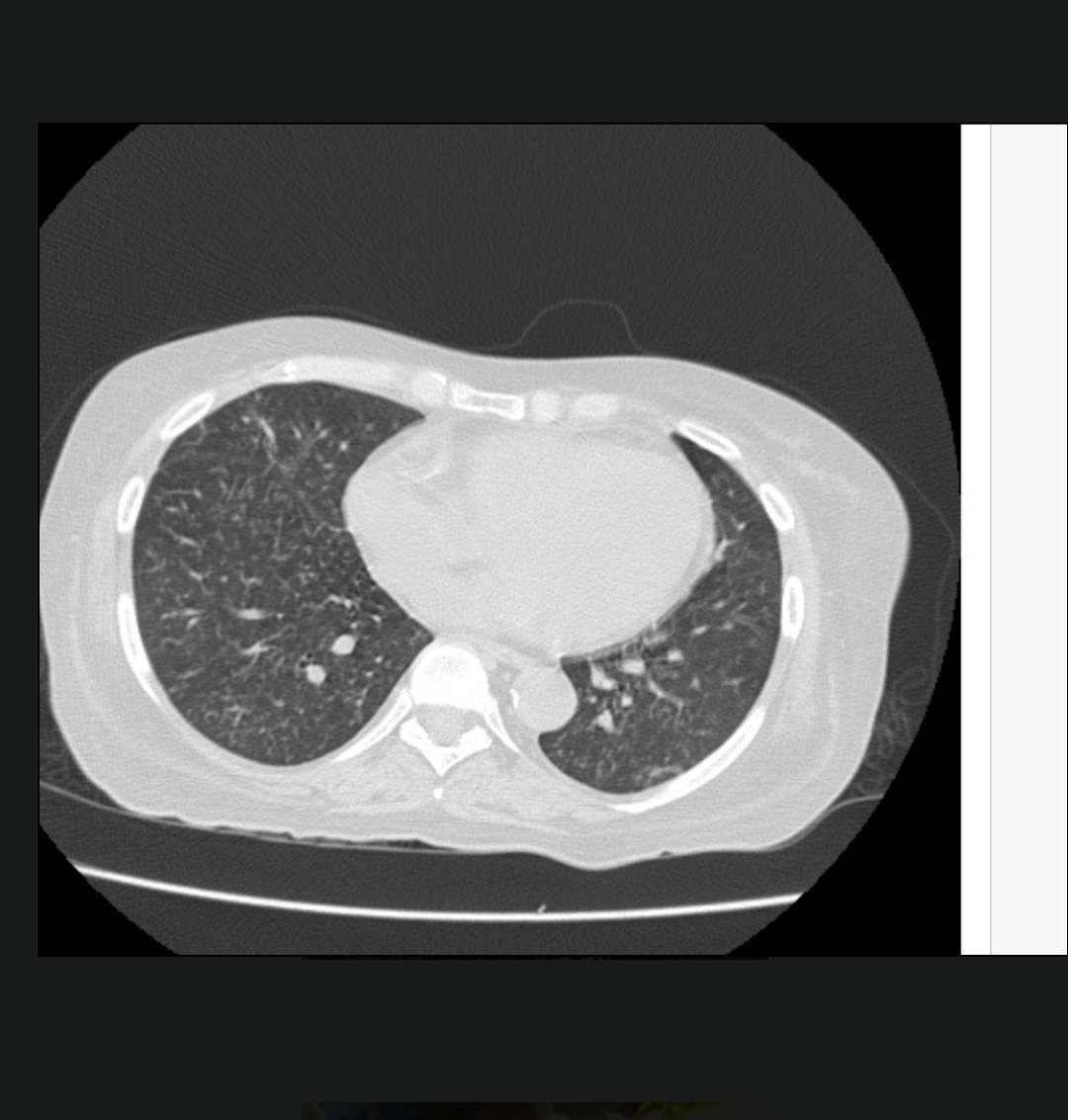
-Few small volume mediastinal lymph nodes noted
-Both lungs are studded with tiny nodular densities - miliary TB or ILD?
-Small air filled cyst noted left lower lobe.
-No evidence of effusion.
-Non-obstructive left renal calculus.
PROVISIONAL DIAGNOSIS :
Miliary tuberculosis , ATT induced scleroderma
K/c/o HTN , HYPOTHYROIDISM
TREATMENT PLAN:
Stop ATT
IVF NS/RL/DNS @ 75 ml/hr
NEB. Ipravent 1resp inH TID
NEB. BUDICORT 1RESP INH TID
INJ. HUMAN ATRAPID according to sliding scale
Inj. PIPTAZ 2.25 gm IV TID
T. Thyronorm 50 mg PO OD
INJ. PAN 40 MG IV OD
T. AMLONG 5 MG PO OD
MUCOPAIN JEL L/A 40 MINS BEFORE MEAL
Betadine mouth wash TID
Liquid paraffin all over body TID






Comments
Post a Comment