A 80y/o male came to casualty in an unresponsive state.
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
Chief complaints:
A 80yr old male patient who rear goat by occupation was presented to casualty in an unresponsive state since 2hrs on 14/09/22.
HOPI:
Patient was conscious, unresponsive
No pallor, Icterus, clubbing, cyanosis, edema , lymphadenopathy
Vitals :
Temp. 98.3°F
BP - 160/90mmHg
PR- 86bpm
CVS- S1 S2 + , loud s2
RS- BAE +
P/A- soft. NT
GRBS -64mg/dl

Chief complaints:
A 80yr old male patient who rear goat by occupation was presented to casualty in an unresponsive state since 2hrs on 14/09/22.
HOPI:
He was apparently asymptomatic one day back then he presented to the casualty in an unresponsive state since 4am associated with profuse sweating.
DAILY ROUTINE:
His day starts at 5am , he Wakes up and sits for a while then he walks his around with goat that he has been rearing. He does his breakfast at 8am, lunch at 3pm sleeps for a while and then rears the goat for a while then , dinner at 7pm . He Sleeps at around 8-9 pm . He wakes in the middle of the night sometimes if he were hungry and eats rice with milk and goes back to sleep.
On the night of incident he had his dinner at 7pm and went to bed around 9. He woke up at 12 and had rice with milk at 12am and went back to sleep. Later at 5 am he woke up hungry and had rice with milk. In a few minutes he fell on to the bed and was asking for help . He was taken to govt. hospital nearby where he was given treated and then referred to our hospital where he presented in an unresponsive state.
Past history :
H/o fever 1 year back which lasted for 1 week it was associated with chills and rigors, cough . He also complained of breathlessness for which he went to local hospital and was given medication for 1 month. The fever subsided and he was doing fine.
No similar complaints in the past . Non alcoholic, non smoker. No h/o drug usage
No c/o SOB , Orthopnea, PND No chest pain / palpitations/syncopal attacks.
H/o fever 20 days back
N/k/c/o HTN /DM/CAV / TB/ EPILEPSY
Personal history:
Diet : mixed
Appetite: normal
Sleep : regular
Bowel and bladder: regular
Addictions: he used to consume alcohol occasionally 90ml whisky during festivals. Stopped consuming alcohol since 2 years
No h/o smoking
DAILY ROUTINE:
His day starts at 5am , he Wakes up and sits for a while then he walks his around with goat that he has been rearing. He does his breakfast at 8am, lunch at 3pm sleeps for a while and then rears the goat for a while then , dinner at 7pm . He Sleeps at around 8-9 pm . He wakes in the middle of the night sometimes if he were hungry and eats rice with milk and goes back to sleep.
On the night of incident he had his dinner at 7pm and went to bed around 9. He woke up at 12 and had rice with milk at 12am and went back to sleep. Later at 5 am he woke up hungry and had rice with milk. In a few minutes he fell on to the bed and was asking for help . He was taken to govt. hospital nearby where he was given treated and then referred to our hospital where he presented in an unresponsive state.
Past history :
H/o fever 1 year back which lasted for 1 week it was associated with chills and rigors, cough . He also complained of breathlessness for which he went to local hospital and was given medication for 1 month. The fever subsided and he was doing fine.
No similar complaints in the past . Non alcoholic, non smoker. No h/o drug usage
No c/o SOB , Orthopnea, PND No chest pain / palpitations/syncopal attacks.
H/o fever 20 days back
N/k/c/o HTN /DM/CAV / TB/ EPILEPSY
Personal history:
Diet : mixed
Appetite: normal
Sleep : regular
Bowel and bladder: regular
Addictions: he used to consume alcohol occasionally 90ml whisky during festivals. Stopped consuming alcohol since 2 years
No h/o smoking
FAMILY HISTORY:
There is no similar complaints in his family.
GENERAL EXAMINATION:
Patient was conscious, unresponsive
No pallor, Icterus, clubbing, cyanosis, edema , lymphadenopathy
Vitals :
Temp. 98.3°F
BP - 160/90mmHg
PR- 86bpm
CVS- S1 S2 + , loud s2
RS- BAE +
P/A- soft. NT
GRBS -64mg/dl

SYSTEMIC EXAMINATION:
CVS- S1 S2 + , loud s2
RS- BAE +
P/A- soft. NT
GRBS -64mg/dl
Provisional diagnosis:
S:
S:
S:
RS- BAE +
P/A- soft. NT
GRBS -64mg/dl
Provisional diagnosis:
recurrent Hypoglycemia resolved ,
Type II respiratory failure. 2° to ? CAP with old ? PTB .
Investigations :
14/09/22
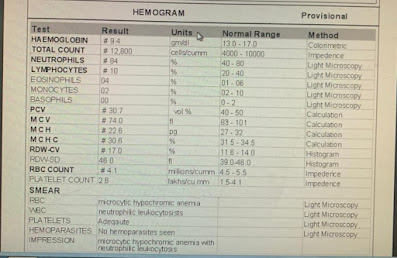
Hemogram

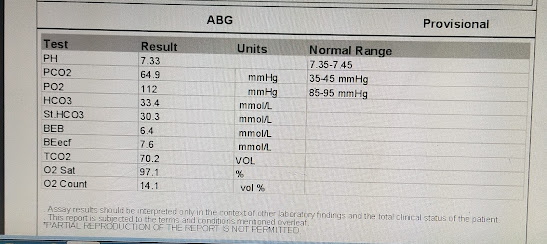
ABG at 9:48am

ABG at 4:40pm

RFT

Chest x-ray

USG

15/09/22
Hemogram
ESR - 20 mm/ 1st hr.
Type II respiratory failure. 2° to ? CAP with old ? PTB .
Investigations :
14/09/22
Hemogram

ABG at 9:48am

ABG at 4:40pm

RFT

Chest x-ray

USG

15/09/22
Hemogram
ESR - 20 mm/ 1st hr.
Serum creatinine - 0.8 mg/dl
Serum electrolytes -
Na- 136mEq/L
K- 3.3 mEq/L
Cl - 0.86 mmol/L
ABG

CUE

15-09-22
Serum electrolytes -
Na- 136mEq/L
K- 3.3 mEq/L
Cl - 0.86 mmol/L
ABG

CUE

15-09-22
Treatment
1) INJ. 25 % DEXTROSE @ 50 ml/ hr (target range
: 120-180mg/dl)
2) NEBULIZATION T DUOLIN 6th hrly, BUDECORT 8th hrly
3) BP, PR, RR, CHARTING 4th hrly.
4) INJ. LASIX 20 mg stat.
16-09-22
1) INJ. 25 % DEXTROSE @ 50 ml/ hr (target range
: 120-180mg/dl)
2) NEBULIZATION T DUOLIN 6th hrly, BUDECORT 8th hrly
3) BP, PR, RR, CHARTING 4th hrly.
4) INJ. LASIX 20 mg stat.
16-09-22
S:
pt. is sedated and paralysed
O :
Pt is , on mechanical ventilator
Temp- 98.0 °F
PR:88bpm
BP:100/60
CVS: S1 S2 +, LOUD S2
RS: BAE+
SpO2 100% ,
TFiO2 - 40
RR- 25
PEEP- 8
I:E- 1:3
Peak - 20
TV -300ml
GRBS- 187 mg/dl ,
P/A: soft , non tender
A: recurrent hypoglycemia 2° ? Insulin auto immune syndrome, ? Sepsis ? PTB
Type 2 respiratory failure 2° to CAP
P:
1)INJ. 25% DEXTROSE @15ml/hr to maintain RBS 120-180mg/dl
2) IVF- NS 30 ml/hr
3) INJ. LASIX 20mgIV/BD
4) RT FEEDS @75ml/2nd hrly
5) INJ. MIDAZOLAM 10ml +40ml NS @ 5ml/hr
6) INJ ATRACURIUM 5ml+ 45ml NS @ 5ml/hr
7) BP/PR/RR/SPO2/GRBS CHARTING
8) AIR BED.
17/09/22
O :
Pt is , on mechanical ventilator
Temp- 98.0 °F
PR:88bpm
BP:100/60
CVS: S1 S2 +, LOUD S2
RS: BAE+
SpO2 100% ,
TFiO2 - 40
RR- 25
PEEP- 8
I:E- 1:3
Peak - 20
TV -300ml
GRBS- 187 mg/dl ,
P/A: soft , non tender
A: recurrent hypoglycemia 2° ? Insulin auto immune syndrome, ? Sepsis ? PTB
Type 2 respiratory failure 2° to CAP
P:
1)INJ. 25% DEXTROSE @15ml/hr to maintain RBS 120-180mg/dl
2) IVF- NS 30 ml/hr
3) INJ. LASIX 20mgIV/BD
4) RT FEEDS @75ml/2nd hrly
5) INJ. MIDAZOLAM 10ml +40ml NS @ 5ml/hr
6) INJ ATRACURIUM 5ml+ 45ml NS @ 5ml/hr
7) BP/PR/RR/SPO2/GRBS CHARTING
8) AIR BED.
17/09/22
SOB improved
O :
Pt is concious , coherent and cooperative
Temp- 99.8°F
PR:91bpm
BP:100/60mmHg
CVS: S1 S2 +
RS: BAE+, NVBS
CNS: NAD
SpO2: 98%
GRBS- 112 mg/dl ,
P/A: soft , non tender
A: recurrent hypoglycemia 2° ? Insulin auto immune syndrome, ? Sepsis ?
Type 2 respiratory failure 2° to ? active PTB ?CAP
P:
1) IVF- NS @ 30 ml/hr
2) INJ. LASIX 20mgIV/BD
3) TAB.ISONIAZID 75mg
TAB.RIFAMPICIN 150mg
TAB. PYRAZINAMIDE 400mg
TAB. ETHAMBUTOL 275mg
(3 TAB PO/OD)
4)BP/PR/RR/SPO2/GRBS CHARTING
5) AIR BED.
22/09/22
O :
Pt is concious , coherent and cooperative
Temp- 99.8°F
PR:91bpm
BP:100/60mmHg
CVS: S1 S2 +
RS: BAE+, NVBS
CNS: NAD
SpO2: 98%
GRBS- 112 mg/dl ,
P/A: soft , non tender
A: recurrent hypoglycemia 2° ? Insulin auto immune syndrome, ? Sepsis ?
Type 2 respiratory failure 2° to ? active PTB ?CAP
P:
1) IVF- NS @ 30 ml/hr
2) INJ. LASIX 20mgIV/BD
3) TAB.ISONIAZID 75mg
TAB.RIFAMPICIN 150mg
TAB. PYRAZINAMIDE 400mg
TAB. ETHAMBUTOL 275mg
(3 TAB PO/OD)
4)BP/PR/RR/SPO2/GRBS CHARTING
5) AIR BED.
22/09/22
SOAP NOTES:
S:
SOB improved
O :
Pt is concious , coherent and cooperative
Temp- 98.0°F
PR:80bpm
BP:110/80mmHg
CVS: S1 S2 +
RS: BAE+
CNS: NAD
SpO2: 92% with 2L of O2 and over night CPAP
GRBS- 80 mg/dl ,
P/A: soft , non tender
A:
Type 2 respiratory failure 2° to ? active PTB ?CAP
Recurrent hypoglycemia resolved, secondary to ? IAS , PTB
P:
1) IVF- NS @ 30 ml/hr
2) TAB.ISONIAZID 75mg
TAB.RIFAMPICIN 150mg
TAB. PYRAZINAMIDE 400mg
TAB. ETHAMBUTOL 275mg
(3 TAB PO/OD)
3)ABG 6TH HRLY
4)BP/PR/RR/SPO2/GRBS CHARTING
5) AIR BED.
24/09/22
O :
Pt is concious , coherent and cooperative
Temp- 98.0°F
PR:80bpm
BP:110/80mmHg
CVS: S1 S2 +
RS: BAE+
CNS: NAD
SpO2: 92% with 2L of O2 and over night CPAP
GRBS- 80 mg/dl ,
P/A: soft , non tender
A:
Type 2 respiratory failure 2° to ? active PTB ?CAP
Recurrent hypoglycemia resolved, secondary to ? IAS , PTB
P:
1) IVF- NS @ 30 ml/hr
2) TAB.ISONIAZID 75mg
TAB.RIFAMPICIN 150mg
TAB. PYRAZINAMIDE 400mg
TAB. ETHAMBUTOL 275mg
(3 TAB PO/OD)
3)ABG 6TH HRLY
4)BP/PR/RR/SPO2/GRBS CHARTING
5) AIR BED.
24/09/22
SOAP NOTES:
S:
SOB improved
O :
Pt is concious , coherent and cooperative
Temp- 98.7°F
PR:104bpm
BP:110/70mmHg
CVS: S1 S2 +
RS: BAE+, B/L basal crepts
CNS: NAD
SpO2: 88%
GRBS- 80 mg/dl ,
P/A: soft , non tender
A:
Type 2 respiratory failure 2° to ? PTB
Recurrent hypoglycemia resolved, secondary to ?sepsis
P:
1) IVF- NS @ 50 ml/hr
2) O2 INHALATION TO MAINTAIN SPO2 >/= 92%
3) TAB.ISONIAZID 75mg
TAB.RIFAMPICIN 150mg
TAB. PYRAZINAMIDE 400mg
TAB. ETHAMBUTOL 275mg
(3 TAB PO/OD)
3) INTERMITTENT BIPAP
4) ABG 6TH HRLY
5)BP/PR/RR/SPO2/GRBS CHARTING
6) INFORM SOS
25-09-22
SOAP NOTES:
O :
Pt is concious , coherent and cooperative
Temp- 98.7°F
PR:104bpm
BP:110/70mmHg
CVS: S1 S2 +
RS: BAE+, B/L basal crepts
CNS: NAD
SpO2: 88%
GRBS- 80 mg/dl ,
P/A: soft , non tender
A:
Type 2 respiratory failure 2° to ? PTB
Recurrent hypoglycemia resolved, secondary to ?sepsis
P:
1) IVF- NS @ 50 ml/hr
2) O2 INHALATION TO MAINTAIN SPO2 >/= 92%
3) TAB.ISONIAZID 75mg
TAB.RIFAMPICIN 150mg
TAB. PYRAZINAMIDE 400mg
TAB. ETHAMBUTOL 275mg
(3 TAB PO/OD)
3) INTERMITTENT BIPAP
4) ABG 6TH HRLY
5)BP/PR/RR/SPO2/GRBS CHARTING
6) INFORM SOS
25-09-22
SOAP NOTES:
S:
SOB improved
O :
Pt is concious , coherent and cooperative
Temp- 97.6°F
PR:74bpm
BP:120/80mmHg
CVS: S1 S2 +
RS: BAE+, B/L basal crepts
CNS: NAD
SpO2: 88%
GRBS- 61mg/dl ,
P/A: soft , non tender
A:
Type 2 respiratory failure 2° to ? PTB (clinico radiographic)
Recurrent hypoglycemia (resolved), secondary to ?sepsis
P:
1) IVF- NS @ 50 ml/hr
2) O2 INHALATION TO MAINTAIN SPO2 >/= 92%
3) TAB.ISONIAZID 75mg
TAB.RIFAMPICIN 150mg
TAB. PYRAZINAMIDE 400mg
TAB. ETHAMBUTOL 275mg
(3 TAB PO/OD)
3) TAB.MET-XL 25mg PO/OD
4) INTERMITTENT BIPAP
5) ABG 6TH HRLY
6)BP/PR/RR/SPO2/GRBS CHARTING
7) INFORM SOS
26/9/22
Pt is concious , coherent and cooperative
Temp- 97.6°F
PR:74bpm
BP:120/80mmHg
CVS: S1 S2 +
RS: BAE+, B/L basal crepts
CNS: NAD
SpO2: 88%
GRBS- 61mg/dl ,
P/A: soft , non tender
A:
Type 2 respiratory failure 2° to ? PTB (clinico radiographic)
Recurrent hypoglycemia (resolved), secondary to ?sepsis
P:
1) IVF- NS @ 50 ml/hr
2) O2 INHALATION TO MAINTAIN SPO2 >/= 92%
3) TAB.ISONIAZID 75mg
TAB.RIFAMPICIN 150mg
TAB. PYRAZINAMIDE 400mg
TAB. ETHAMBUTOL 275mg
(3 TAB PO/OD)
3) TAB.MET-XL 25mg PO/OD
4) INTERMITTENT BIPAP
5) ABG 6TH HRLY
6)BP/PR/RR/SPO2/GRBS CHARTING
7) INFORM SOS
26/9/22
SOAP NOTES:
S: Pedal edema
Thrombophelbitis
SOB improved
O: Pt is conscious,coherent
Cooperative
BP-100/60
Pr-74bpm
Temp-Afebrile
RR- 16cpm
CVS-S1S2+
P/A -soft,NT
A:
Type 2 respiratory failure secondary to? PTB(clinicoradiological)
Recurrent hypoglycemia (resolved)
secondary to ? Sepsis
P:plan for treatment
1.Tab lasix 40mg/PO/OD
2.Oral fluids@ 1-1.5l
3.O2 inhalation to maintain Spo2- >92%
4.INTERMITTENT BIPAP
5.TAB MET-XL 25mg/PO/OD
6.TAB RIFAMPICIN 150mg
TAB ISONIAZID 75mg
TAB PYRAZINAMIDE 40mg
TAB ETHAMBUTHOL 275mg
(3TAB PO/OD)
S: Pedal edema
Thrombophelbitis
SOB improved
O: Pt is conscious,coherent
Cooperative
BP-100/60
Pr-74bpm
Temp-Afebrile
RR- 16cpm
CVS-S1S2+
P/A -soft,NT
A:
Type 2 respiratory failure secondary to? PTB(clinicoradiological)
Recurrent hypoglycemia (resolved)
secondary to ? Sepsis
P:plan for treatment
1.Tab lasix 40mg/PO/OD
2.Oral fluids@ 1-1.5l
3.O2 inhalation to maintain Spo2- >92%
4.INTERMITTENT BIPAP
5.TAB MET-XL 25mg/PO/OD
6.TAB RIFAMPICIN 150mg
TAB ISONIAZID 75mg
TAB PYRAZINAMIDE 40mg
TAB ETHAMBUTHOL 275mg
(3TAB PO/OD)













Comments
Post a Comment